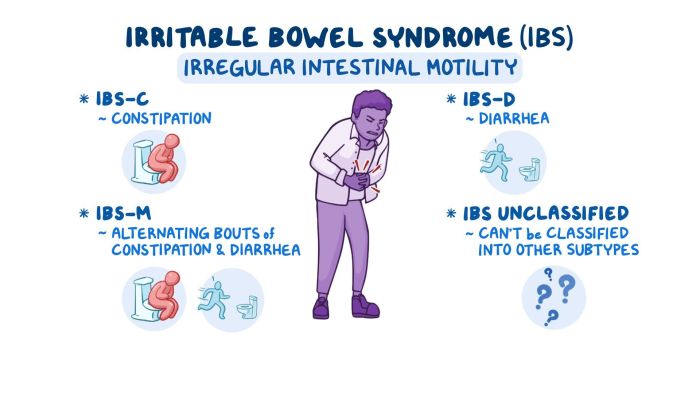
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by abdominal pain, cramping, bloating, and altered bowel habits. The irritable bowel syndrome nursing diagnosis plays a crucial role in guiding patient care and improving outcomes. This article provides a comprehensive overview of the nursing assessment, interventions, patient education, interprofessional collaboration, and evaluation process involved in IBS management.
IBS affects approximately 10-15% of the population worldwide, with a higher prevalence in women. The exact cause of IBS is unknown, but it is believed to involve a combination of factors, including altered gut motility, visceral hypersensitivity, and psychological distress.
Nursing Assessment: Irritable Bowel Syndrome Nursing Diagnosis
The nursing assessment for irritable bowel syndrome (IBS) involves gathering subjective and objective data to establish a comprehensive understanding of the patient’s symptoms, medical history, and lifestyle factors.
Subjective Data, Irritable bowel syndrome nursing diagnosis
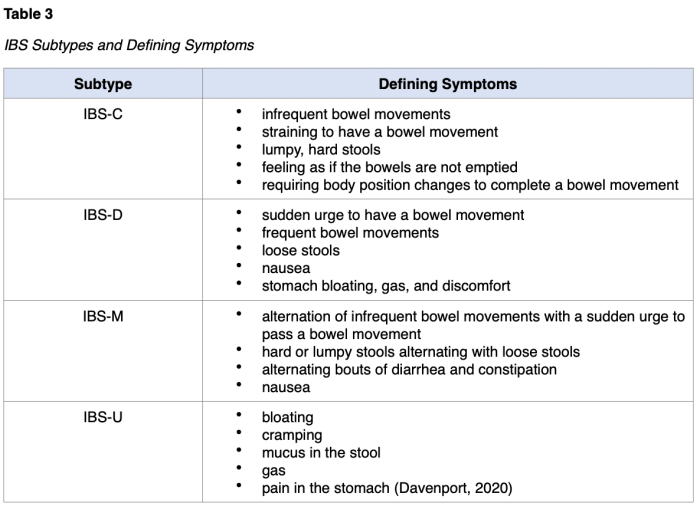
- Symptoms: Character, frequency, severity, and duration of abdominal pain, bloating, diarrhea, and constipation
- Bowel habits: Changes in stool consistency, frequency, and urgency
- Dietary patterns: Foods that trigger or alleviate symptoms
- Stress levels: Perceived stress and its impact on symptoms
- Sleep quality: Sleep disturbances and their relationship to IBS symptoms
Objective Data
- Physical examination: Abdominal palpation, auscultation, and percussion to assess for tenderness, distension, and borborygmi
- Laboratory tests: Stool analysis, blood tests, and imaging studies to rule out other conditions
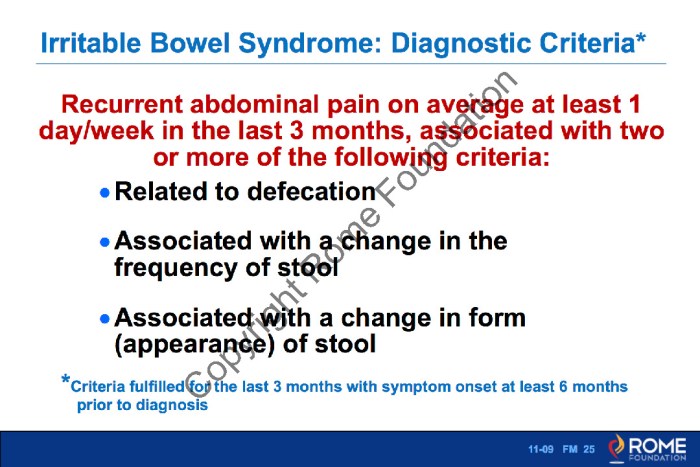
Diagnostic Criteria
IBS is diagnosed based on the Rome IV criteria, which include:
- Recurrent abdominal pain at least one day per week for the past three months
- Symptoms that have been present for at least six months
- Symptoms that are relieved by defecation
- Symptoms that are associated with a change in stool form or frequency
Nursing Interventions
Nursing interventions for IBS focus on managing symptoms, improving quality of life, and providing patient education.
Symptom Management
- Dietary modifications:Advising patients to avoid trigger foods and follow a low-FODMAP diet
- Stress management techniques:Teaching relaxation techniques such as deep breathing and meditation
- Medication:Prescribing antispasmodics, antidiarrheals, and laxatives as needed
Quality of Life Improvement
- Sleep hygiene:Promoting regular sleep patterns and a conducive sleep environment
- Exercise:Encouraging regular physical activity to reduce stress and improve digestion
- Emotional support:Providing a supportive environment and connecting patients with support groups
Expected Outcomes
- Reduced abdominal pain and bloating
- Improved bowel function
- Increased quality of life
- Enhanced coping mechanisms
Patient Education
Patient education is crucial in IBS management. It empowers patients to self-manage their symptoms and improve their overall well-being.
Topics covered in patient education include:
- Understanding IBS and its symptoms
- Trigger identification and avoidance
- Dietary modifications
- Stress management techniques
- Medication adherence
- Symptom monitoring and reporting
Patient Education Materials
- Patient handouts and brochures
- Online resources and support groups
- Personalized education plans developed by healthcare providers
Interprofessional Collaboration
Interprofessional collaboration is essential in IBS management to provide comprehensive care and improve patient outcomes.
Healthcare professionals involved in IBS care include:
- Primary care physicians
- Gastroenterologists
- Registered dietitians
- Mental health professionals
Collaboration involves:
- Sharing patient information and perspectives
- Developing and implementing individualized treatment plans
- Monitoring patient progress and adjusting interventions as needed
Evaluation
Evaluation of nursing interventions for IBS is essential to assess their effectiveness and guide ongoing care.
Indicators used to measure effectiveness include:
- Frequency and severity of abdominal pain
- Bowel function and stool consistency
- Quality of life measures
- Patient satisfaction
Ongoing evaluation allows nurses to:
- Identify areas for improvement
- Adjust interventions to meet changing patient needs
- Optimize patient outcomes
FAQ Insights
What are the common symptoms of IBS?
Abdominal pain, cramping, bloating, diarrhea, constipation, alternating diarrhea and constipation, and urgency to defecate.
How is IBS diagnosed?
IBS is diagnosed based on the Rome IV criteria, which include recurrent abdominal pain for at least 1 day per week for the past 3 months, associated with two or more of the following: improvement with defecation, onset associated with a change in stool frequency, and onset associated with a change in stool form.
What are the goals of IBS management?
The goals of IBS management include reducing symptoms, improving quality of life, and preventing complications.
What is the role of the nurse in IBS management?
Nurses play a crucial role in IBS management by providing patient education, administering medications, monitoring symptoms, and collaborating with other healthcare professionals.